Last month saw the publication of the International Longevity Centre’s (ILC) report ‘Dementia and Comorbidities: Ensuring parity of care’, which shows that people with dementia are less likely to have cases of depression, diabetes or urinary tract infections diagnosed, and those that do are less likely to receive the same help to manage and treat these comorbidities. This lack of parity can lead to people’s dementia worsening more quickly, leading to greater health and social care costs.
So why are we discussing this in a nutrition blog?
The ILC report highlights nutrition issues in the context of both the prevention and management of comorbidities of dementia and diabetes in older people.
Dementia and risk of developing diabetes
Risk factors for type 2 diabetes include obesity, and poor dietary and physical activity patterns. Studies have shown that the onset of dementia may make some people more susceptible to risk factors for diabetes as it can lead to changes in appetite, food preferences, and eating habits. For example, while undernutrition is generally a greater problem for people with dementia, it can also lead to a person developing a preference for sweet foods or savoury high fat/salty snacks which can have higher calorie content with an adverse impact on weight management. Frontotemporal dementia in particular has been shown to lead to a greater intake of sugar and carbohydrates. Additionally, older people with greater cognitive impairment are less likely to adhere to a recommended diet.
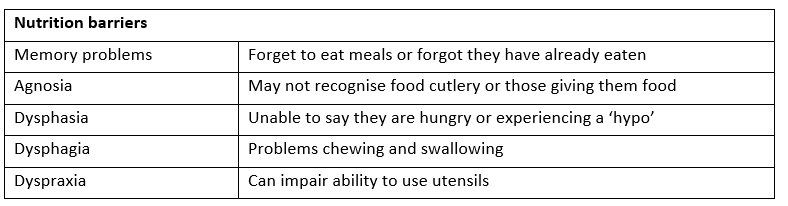
Barriers to healthy eating in people with diabetes and dementia include the following:
Management and treatment
There are no national clinical guidelines that specifically make reference to the management of diabetes in people with dementia. Yet the high prevalence of diabetes in the UK (over 3 million people) means that many people who develop dementia will already have diabetes, and have had some experience of the management and treatment of diabetes.
However changes that occur in dementia, particularly around decline in memory function, can lead to difficulties with self-management. For example:
- Forgetting to take medications, with risk of missing medication or double dosing;
- Forgetting how to administer injections;
- Becoming unable to make decisions about interpreting blood glucose results;
- Missing meals and drinks so at risk of low blood glucose levels and dehydration;
- Forgetting they have eaten and at risk of high glucose levels if they eat again.
Issues for people with dementia who develop diabetes
These problems may be more amplified for people who develop diabetes after being diagnosed with dementia, as they have no prior experience of self-managing the disease. This puts them at even greater risk of a range of problems including:
- Increased confusion if blood glucose levels are high and causing dehydration;
- Distress if their usual diet is changed significantly;
- Developing incontinence as they need to pass urine more often but may not be able to find the toilet and Increased risk of falls due to more frequent visits to the toilet.
The level of support required will vary depending on the severity of the dementia, with research finding that people with diabetes and low levels of cognitive function require significantly more assistance with personal care behaviour than people with diabetes alone.
Carers
Caregivers play a vital role in ensuring that issues highlighted above are addressed and that diabetes is appropriately managed.
Memory loss is often the first sign of self-care neglect, leading to a need for caregiver intervention to help a person with dementia manage their diabetes. However, caregivers face a number of challenges and quality-of-life issues. The behavioural and psychological symptoms of dementia often disrupt the daily diabetes care routine, such as a ‘denial’ of having diabetes or memory loss.
Case Study
One of the most rewarding aspects of reading The ILC report was the real life illustrative ‘good’ care stories. For diabetes and dementia the illustrative case was Mrs Green in a nursing home.
Mrs Green’s story – Good Practice example
Background
- Age 83;
- Type 2 diabetes for 30 years;
- Dementia for 2 years;
- Recent admission to nursing home.
Mrs Green
Mrs Green had been self-managing her condition well. However, as her dementia progressed she had:
- Forgotten to take her medications;
- Experienced a series of hypos;
- Found it increasingly hard to interpret her blood glucose results;
- Forgotten to eat regular meals and had lost weight.
Mrs Green’s GP
Mrs Green’s GP developed a support plan to communicate to the nursing home. This included:
- Agreed safe blood glucose targets;
- Recommendations for her diet;
- Prompts to arrange an annual diabetes check-up to monitor her blood glucose levels, cholesterol levels and vision.
Nursing home staff
On admission, the staff discussed with Mrs Green and her daughters how she had conducted diabetic procedures in the past. Her daughters were able to fill in the gaps where Mrs Green couldn’t remember.
This helped Mrs Green in being familiar with the regime for her blood glucose monitoring and insulin administration. Staff also initiated a number of strategies to maximise her dietary intake, including:
- Serving one course at a time to reduce confusion;
- Allowing extra time for her to return to her meal;
- Encouraging dairy products as snacks when other foods were refused.
The result of these measures was Mrs Green’s blood glucose levels were adequately controlled, and she rarely experienced any distress when her daily diabetes management routine was being carried out.
Recommendations from the report
Two of the recommendations from the ILC report directly related to care homes.
- Care homes should modify the care plans of residents with dementia to include checklists covering the symptoms of common comorbidities to help ensure early diagnosis and treatment.
- The Care Quality Commission (CQC) should consider making it mandatory for care homes to undertake annual check-ups for residents with dementia and diabetes where their blood glucose levels, cholesterol levels and vision are monitored.
Perhaps such measures will help towards ensuring parity of care for people with the comorbidities of dementia and diabetes.