At the end of last year, the British Association for Parenteral and Enteral Nutrition (BAPEN), a charitable association that raises awareness of malnutrition, published its Nutrition Screening Week Care Home Reports.
At the end of last year, the British Association for Parenteral and Enteral Nutrition (BAPEN), a charitable association that raises awareness of malnutrition, published its Nutrition Screening Week Care Home Reports.
Summary of the BAPEN’s findings
The published reports contain amalgamated data obtained from the care homes that participated in BAPEN’s four UK Nutrition Screening Weeks ((NSW) which took place between 2007 and 2011. The NSW surveys involved a total of 474 care homes, and 3971 adult residents in the UK. The majority of data were provided from care homes in England and to a progressively smaller extent from those in Scotland, Wales and Northern Ireland. The results suggest that ‘malnutrition’ (defined as medium + high risk according to the ‘MUST’ nutrition screening tool) is common within care homes, with a prevalence of about 35% among residents admitted in the previous 6 months.
Apart from providing a comprehensive analysis of the amalgamated data obtained from care homes, the reports provide a variety of new information. This includes trends in nutritional care over time, and an analysis of the weight changes that occur in care homes during the six months after admission. It also reports on comparisons between England and the rest of the UK, and between care homes and the general population.
What did the reports find?
Prevalence of ‘malnutrition’ did not differ significantly between England, Scotland, Wales and Northern Ireland. It varied with disease category, and was higher in residents with cancer than those without and in those suffering from multiple rather than a single condition.
It was also reported that ‘malnutrition’ was:
- Lower (27%) in residents who had been admitted into exclusively residential care homes than all other types of care homes (38%). This may be because residents in the other types of care homes, especially nursing homes, are expected to have more severe disease.
- Lower in those admitted from their own homes (30%) than from hospitals (39%) and other care homes (37%). This may reflect the type and severity of disease likely to predispose to or be the result of ‘malnutrition’ and vice versa.
- Lower in men than in women (30 vs 38%).
- Lower in younger than in older residents (27% in those <75 years, 39% in those 70-84 years, and 39% in those ≥85 years).
Residents who were malnourished on admission to care were more likely to lose further weight during their residency, while those at low risk of malnutrition gained weight. Most residents who were underweight on admission remained underweight at the time of the survey.
Care home residents compared to the general population
In comparison with the general population, care home residents were much more likely to be underweight (BMI < 20 kg/m2). The frequency of underweight in care home residents was found to increase strikingly with age. In contrast, obesity was distinctly less common among care homes than the general population (9 vs 28%). This is likely to be because care home residents typically have poorer health status, have greater and more severe disease presence, and are more likely to have dementia and frailty than older people in the general population.
Nutrition practice in care homes
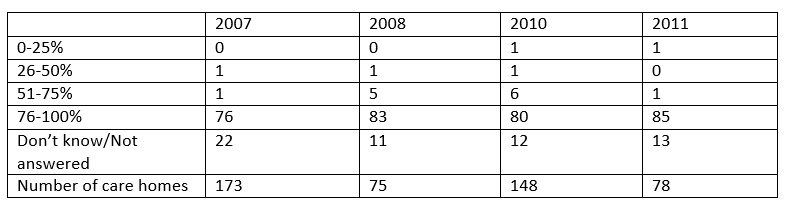
The authors suggest that during the five year period there was some evidence of improvements throughout the UK in terms of awareness of ‘malnutrition’, in nutritional screening practice. The table below, for example, illustrates a rising trend in the proportion of residents screened on admission, and the vast majority of care homes reported linking the results of screening to a care plan.
Table showing the proportion of residents screened on admission.
In addition trend analysis of consecutive surveys indicated that the majority of care homes routinely weighed residents on admission and during their stay and that there were significant improvements in the recording of height on admission, and access to dietetic services.
However, there was room for improvement in some aspects of nutritional care, such as awareness of the existence of weighing scale standards and undertaking audits on nutritional screening.
BAPEN summary of malnutrition in care homes
The reports indicate that ‘malnutrition’ in care homes is a major health and social care burden. While care homes are generally funded to provide social care, the boundaries between social and health care are ill defined and sometimes problematic, suggesting that more integrated health and social care strategies to combat the problems would be beneficial. The care home surveys suggest that there have been some improvements in the operational infrastructure for the management of ‘malnutrition’, but there is still room for further improvement, in line with the conclusions of the Dignity and Nutrition Inspections of care homes undertaken by the Care Quality Commission.