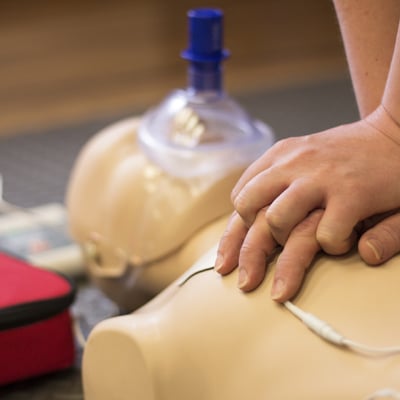
The medical decision of ‘Do not attempt Cardio-pulmonary resuscitation’ (DNACPR) is a plan discussed with patients and their carers in advance, as to how to treat an irreversible and terminal illness in the event of their pulse and breathing stopping. It is an essential guide for health practitioners in the relevant situations, and can provide reassurance to patients that a resuscitation (CPR) process will not be carried out where it is unlikely to succeed, or to cause harm and distress to the patient.
The Scottish Health Minister recently introduced a new policy on CPR, based on updated best practice in health care provision across the UK.
The Minister said that:
“Whether or not to attempt CPR towards the end of someone’s life is one of the most emotive and sensitive decisions that patients, doctors and relatives will ever have to face and this policy identifies the key importance of conversations with patients and families. Supporting staff in all health and social care settings to have these sensitive discussions is of the utmost importance.
“Treatment options must be discussed honestly and the patient’s wishes must be taken into account where possible. The option of a dignified death must be open to everyone in all circumstances.”
New Additions to the Previous Versions of the Cardio-Pulmonary Resuscitation Policy (CPR)
The Government website gives the following, but NB the full policy should be read for information:
1 When it is clear in advance that CPR will not be successful there should be a presumption in favour of informing patients of a DNACPR decision. This information should always be shared sensitively in the context of exploring their goals of care and wishes around realistic emergency treatment options.
2 When CPR will not be successful and a DNACPR decision has been made and documented, the only justification for not sharing this information with a patient is:
KEY POINTS – these points emphasise new and commonly misunderstood aspects of the DNACPR policy but should not be read in exclusion from the policy document.
- The patient lacks capacity to engage with that conversation (information must be shared with the welfare attorney/guardian or relevant others as soon as possible where this is practicable and appropriate);
- The patient refuses to engage with that conversation (ask if there is anyone that the patient would give the clinical team permission to talk with about important healthcare issues?);
- It is judged that the conversation would cause the patient physical or psychological harm.
3 Where a clinical team is as certain as it can be that CPR will not be successful and that the patient is irreversibly deteriorating, the DNACPR decision will remain appropriate until the patient’s death and does not need reviewed. However, senior clinicians taking over clinical responsibility for the patient (transfer or discharge to a different team) should still review the decision and document that they are in agreement.
Points for Care Services
I came across anecdotal evidence of poor practice in this area in the past, where decisions were made inappropriately not to resuscitate, or without advance discussion with the patient or their representative.
I think services should be clear on how this new policy should be implemented and discussed, to ensure that people using the services have their rights to dignified and safe end of life medical care provision.