I was inspired to write this article after a recent experience in practice where a patient accidentally swallowed a scaler tip. I wanted to share this experience to:
- Inform dental managers and teams on the necessary steps to follow in the event of an incident
- To establish how we respond to an incident to mitigate future risk
Patients trust dental professionals to carry out procedures often involving very small or sharp instruments. Theses are sometimes hazardous materials that are a choking hazard and this all takes place whilst they are reclined back in a dental chair with their mouths wide open.
Foreign body ingestion is a well known but often overlooked risk of dental treatment. The majority of the risk is associated with handling very small instruments such as root canal files or drill burs in a very small cavity with limited access and poor direct vision.
These adverse incidents are rare but carry a huge risk of trauma, anxiety, and potential harm to the patient. This could also result in a negligence claim against the dental professional. Managing and mitigating the risk is the only way to avoid potential negligence claims and protect the brand and reputation of the practice.
How?
We are a VT training practice and have the absolute pleasure of mentoring newly qualified dentists for their first year in NHS general practice where they get to experience the real world of dentistry at first hand.
During a call back procedure for an AGP RSD appointment, the patient swallowed a scaler tip!
The dentist’s recollection of the event was that they had followed all their necessary steps for assembling the ultrasonic handpiece, they had used the DTE key to tighten the scaler tip on to the body of the ultrasonic handpiece and this was observed by the assisting nurse.
The dentist ran the ultrasonic scaler on the bracket table tray for the required 20 seconds to clear the water lines. But as they began to scale the lower left-hand quadrant, they felt the tip begin to spin and immediately retracted the handpiece. Unfortunately, it was too late, and the scaler tip had detached in the patient’s mouth and was laying between the lingual surface of the back molars and the patient’s tongue.
The nurse acted quickly and used the high-volume suction to try and retrieve the scaler tip while the dentist grabbed the tweezers, but it was too late – the patient reactively swallowed and the scaler tip disappeared down their throat! Both the nurse and dentist reported that this happened so quickly, they barely had time to think, let alone act!
The patient was sat up immediately and asked to rinse out, engage in a cough and shake off their clothing to ensure it was not present but there was no sign of the instrument. The patient was unaware that he had swallowed the object due to the effects of the anaesthetic from the ID block.
This has happened, now what do you do?
- Use of rubber dam or throat gauze should be used wherever clinically possible. Where it is not possible, high volume suction should be used
- Attempt to retrieve the instrument with high volume suction or tweezers
- Sit the patient up and encourage rinsing and coughing, shake off clothing
- Duty of candour – speak to the patient, be open and transparent with them, full disclosure is required
- Observe the patient to ensure vital signs are unaffected – and manage the situation based on the risk – is their breathing laboured? Uncontrollable coughing, choking or gagging? If so, call 999 for an ambulance and prepare to call for urgent help within the team
- If stable, call NHS 111 or the A&E department for advice regarding an X-ray and write a referral letter explaining what happened and what was swallowed or inhaled
- If the patient refuses to attend hospital, document this and advise them of red flag symptoms to look out for at home
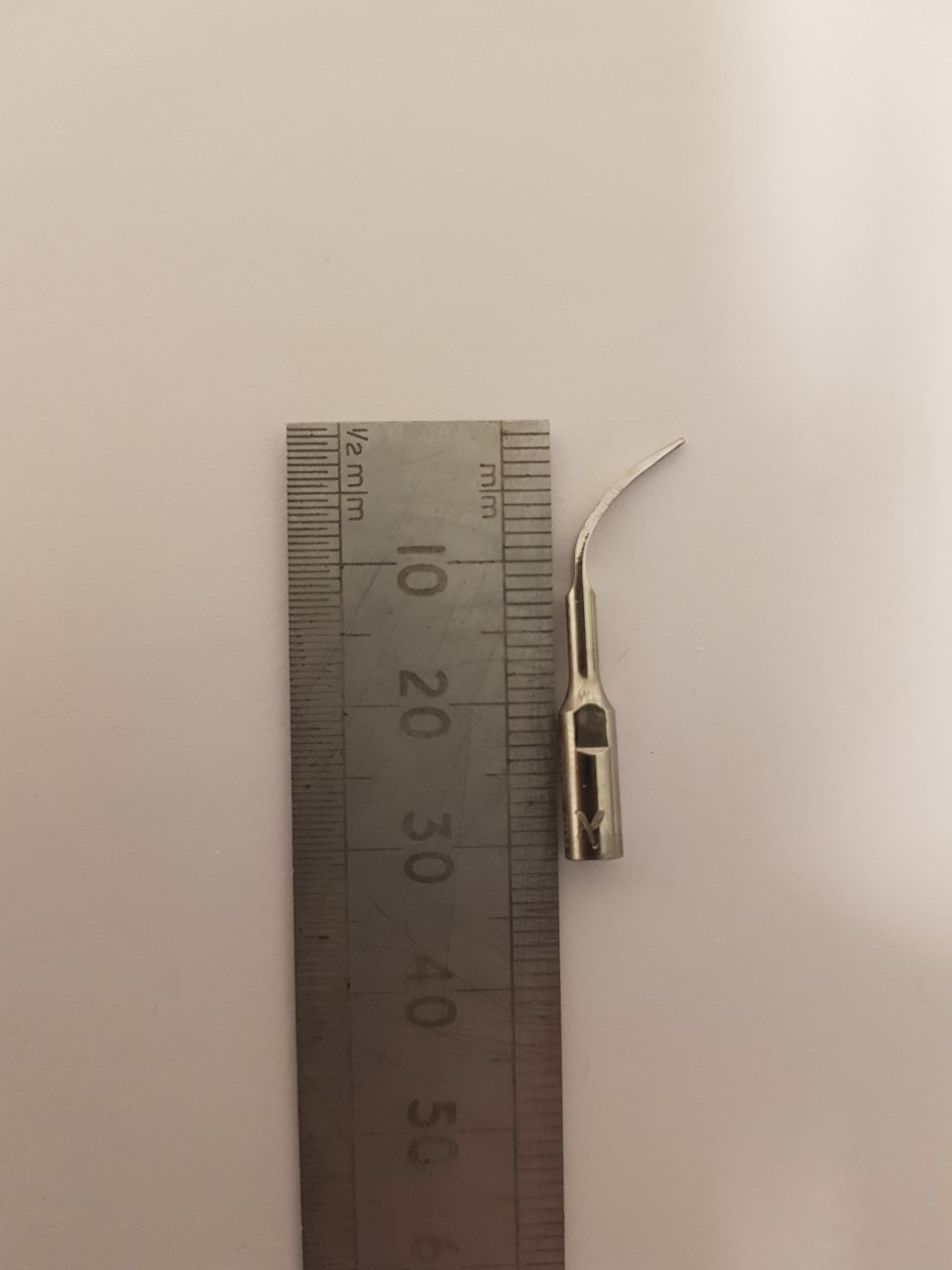
- Take a photograph of a similar scaler tip along side a ruler for size reference and attach to the referral letter
- Stay in touch with the patient, make regular courtesy calls to follow up and reassure the patient that you care
- Call your indemnity provider for advice and follow their guidance on the next steps
- The incident should be recorded in the significant events folder with all the information attached
- Comprehensive records must be made in the patient’s clinical notes
- Witness statements must be obtained from all involved to log in the significant events folder
- Keep a copy of the referral letter and photograph attached in the significant event log in the ‘in progress’ section of the folder for 28 days
- After the 28 days, if the patient reports no further or subsequent health issues associated with the incident, the case can be signed off and closed. However, if there are further health implications directly linked to the incident, this must be reported to the CQC as a reportable incident
- Hold a practice meeting to discuss as a team what happened and look for learning outcomes to action and implement to avoid recurrence in future
- Follow up on your action plan; did you audit instruments and procedures? Did you have training? Consider role playing the situation as a team and having a practice run
- Document it all; if it isn’t written down, it didn’t happen
It is essential that you hold a practice meeting to discuss the incident and to propose learning objectives and how risks could be mitigated. This is what we did, and it was invaluable.
Stay calm during the situation
- Remaining composed allowed the patient to feel calm. Panicking during this time would have only created a more traumatic experience for all involved
- Taking control of the situation immediately demonstrated and modelled to the patient that all was under control. However, unbeknown to him, under the surface we were all nervous wrecks
- We immediately rang 111 and they put us through to our local A&E department where we were able to speak to the on-call doctor. The dentist drafted a letter of referral that was handed to the patient for an urgent x-ray
- Thankfully, two days later, the scaler tip made its grand entrance back into the world the opposite end it went in, and the patient suffered no long-lasting damage!
Action Plan
These are the documented steps that we took:
- We held a wellbeing meeting with the Foundation Dentist, to reassure and support them through their anxieties surrounding the incident – and planned several confidence building tutorials around the incident
- We carried out role play/scenario-based training as a team – documented in the training folder
- We undertook a risk assessment – the clinical team decided on a basic command to confirm the scaler tip has been assembled correctly by carrying out the following:
- the dentist will assemble and tighten the scaler tip on to the ultrasonic handpiece
- the dentist will verbalise this to their nurse by saying ‘scaler tip – checked’
- the nurse will recognise this statement – and confirm back with a ‘yes’ or ‘no’ answer
- if they respond with ‘NO’ then the dentist will re- check that the scaler tip is definitely on tight and reconfirm the verbal statement
- We reviewed the Rubber Dam Policy and Procedure and carried out some further training in Rubber Dam placement
- We created an audit of all the scaler tips and ultrasonic handpieces to ensure quality assurance continuity, ensuring all scaler tips threaded on and tightened sufficiently and disposed of all faulty instruments; this was documented
- We re-ordered scaler tips/ handpieces as necessary
- We have planned to cover inhalation of foreign objects at the next Medical Emergency training
Image of identical scaler tip
What did we learn from this incident?
We learnt that the rare risk is a very real risk and, to be honest, a very scary one. However, in spite of the fear, we managed the situation in a calm and diligent way, avoiding panic and chaos.
We are extremely grateful and thankful that our patient suffered no injuries, other than the inconvenience of a hospital trip and a nervous 15 minutes in the lavatory two days later.
We feel very thankful that our patient was very kind, empathetic and understanding despite the fact he just unknowingly swallowed a sharp dental instrument. We are very aware that the patient’s response to the incident made the overall ordeal far less stressful than if it happened to a dental phobic or anxious patient, or a patient who felt the treatment they received was a result of negligence. Word of mouth can be very harmful in terms of a damaged reputation, especially in a relatively small town. So careful management of the situation was needed to ensure a satisfactory outcome for all involved.
Useful QCS policies
- DAB30 -Significant Event Policy and Procedure
- DME03 – Dental Equipment Maintenance Policy and Procedure
- DAB29 – Duty of Candour Policy and Procedure
- DCH09- Equipment Safety Policy and Procedure
- DHR01- Risk Assessment Policy and Procedure
- DCR02 – Risk Management Policy and Procedure
- DHS18 – Rubber Dam Policy and Procedure
- DHS08 – Serious Incident Notification Policy and Procedure